The Impact of Legal Procedures on Hospital Length of Stay: Balancing Legal and Clinical Concerns
Article information
Abstract
Purpose
Psychiatric hospital length of stay (LOS) is not affected solely by socio-clinical factors but also by legal procedures. This study examined the associations between legal procedures and LOS.
Methods
Data from 521 patients with psychiatric illnesses hospitalized over 2013-2015 were analyzed. Logistic regression was used to evaluate the predictors of longer (> 14 days) or prolonged (> 30) LOS with socio-clinical factors and legal procedures including court-ordered interventions (assisted outpatient treatment, medication over objection, and retention).
Results
Longer LOS occurred in 246 patients and 99 had prolonged LOS. Legal procedures affected 57 patients, with 11 assisted outpatient treatments, 39 cases of medication over objection, and 16 retentions. Longer LOS was significantly associated with six factors including older age, unmarried status, non-Hispanic race, risk of violence, schizophrenia, and legal procedures. Legal procedures had the strongest association. Longer/prolonged LOS yielded qualitatively similar associations.
Conclusion
Among 521 psychiatric inpatients, approximately 11% were mandated to receive interventions/procedures by the courts. Court-ordered legal procedures were strongly associated with longer LOS. Mental health providers may consider legal procedures for patients at high treatment/ medication noncompliance risk as early as patient admission to inpatient units to prevent, intervene or prepare for a longer or prolonged LOS.
INTRODUCTION
In many countries, the managed healthcare model has sparked concern about length of stay (LOS) in acute psychiatric hospitals relative to cost. Against strong forces aimed to reducing inpatient LOS to control psychiatric treatment costs, mental health care providers are challenged to expedite discharges while simultaneously providing optimal care. This conundrum is even more pronounced when carrying for patients with severe mental illness who do not adhere to treatment plans due to a number of reasons related to patient education, side effects, access, and outpatient support. Repeated noncompliance can lead to psychiatric breaks and recurrent return to inpatient care, adding to LOS and/or costs [1-4].
Several studies have explored patient and illness-related factors that contribute to LOS in mental health facilities. A Korean study found that male patients with schizophrenia stayed longer in psychiatric inpatient hospitals than their female counterparts [5]. Other sociodemographic variables including age, marital status, education, employment, and distance between patients' residence and hospital have also been associated with LOS [6-14]. Clinical factors such as a primary diagnosis of schizophrenia and a greater number of previous admissions predicted longer LOS [5-10]. Studies have reported that the presence of substance use disorder is related to shorter LOS, while psychotic or affective disorders are associated with longer LOS [6,7,10]. Other studies, however, suggest that psychopathological symptoms at admission only minimally explain length of inpatient stay [11,12]. On the contrary, complex medical comorbidity has been cited as a contributing factor to prolonged LOS among patients with mental illness. For example, when comorbidity was a focus of care during hospitalization, LOS was prolonged on average by more than 3 days [14]. Moreover, medical comorbidity was associated with a >10% increase in psychiatric symptoms and functional impairment at discharge, even after adjusting for clinical status at admission [14].
Some studies utilized a comprehensive set of static vs. dynamic or external vs. internal factors to better understand the mechanism of LOS [5-7,15-22]. Factors external to patients or providers such as insurance coverage, reimbursement policies, and institutional characteristics have been shown to influence LOS. Provider-level factors, regional characteristics, hospital type, service-level factors, and case-mix were also associated with variations in length of hospitalization [15-22]. An Australian study by Zhang et al. asserted that LOS at an acute psychiatric inpatient unit can be predicted using a multifactorial approach; in particular, behavioral manifestations of illness and lack of social support structures are critical. They also claimed that good clinical practice did not necessarily translate to shorter LOS, where it is not readily modifiable; thus, raising a question about the validity of using rate of readmission as an outcome or quality metric of psychiatric inpatient care, which is often considered together with LOS in health policy [21].
Research on inpatient psychiatric LOS can be further complicated by the inter-relationships between psychopathological, psychosocial, economic, and legal factors [11,23-26]. Although LOS in acute psychiatric hospitals has been extensively studied in terms of characterization, association, and prediction, few studies investigated the potential role of court-mandated interventions or legal factors, including assisted outpatient treatment (AOT), medication over objection (MOO), and retention for court. AOT is indicated for individuals with severe mental illness who meet strict legal criteria, e.g., patients with a history of medication noncompliance, violence, arrest, or two previous psychiatric hospitalizations [6,12,24-26]. Particularly as the most directly relevant and comparable study, Russ and John reported that patients who underwent court-ordered MOO had a longer average LOS that was often accompanied by additional complications throughout medical care and after discharge [24]. Their study comprised 351 patients in 3 groups of MOO, comparison, and control, wherein the principal outcome measures were successful linkage after discharge, readmission within six months of discharge, and transfer to a state hospital, while LOS was described secondarily or exploratorily, without further analyses.
In the current study, we were primarily interested in whether court-ordered interventions or legal procedures are associated with longer LOS adjusting for sociodemographic and clinical factors, with an examination of the relative magnitude of the associations and how much longer.
METHODS
1. Research Design
A retrospective review of medical records and charts was conducted with 521 patients with psychiatric diagnoses hospitalized at a large public hospital providing inpatient psychiatric services on five units, offering acute and short-term treatment in New York City. This study was approved by the Institutional Review Board.
The initial sample size (N) proposed was 400, based on a numerical calculation. Assuming 7% of subjects under court-ordered treatment, we would be able to detect an 8 day difference in the 2 group comparison − 7%:93% for with:without court involvement − with 86% power via a two-sided test where standard deviation (SD) is assumed to be 13, and 5% type-1 error. If we would observe a 5 day difference as a conservative scenario, power would be as low as 46%. Thus, we selected N=600 as our sample size, say, 200 for each of 3 years, in the IRB-approved version of the study (Application #: 16-833 & IRB #: 17-00836). However, owing to limited funding and resources, we had to pause sample selection after 521 patients, which is our final N, still being within the range of 400~600.
2. Patient Population and Data Collection
Data were collected from medical records and chart reviews by psychiatric nurses and psychiatric social workers. A systematic sampling was conducted by selecting every 15th medical record in the years 2013, 2014, and 2015 toward an unbiased and representative sample. For patients with multiple admissions, the first admission was selected for our study. The research team removed personal identifiers and assigned a pseudo identifying number to each chart to preserve confidentiality.
Data were collected from 521 patients who are 18 years old or older with a Diagnostic and Statistical Manual (DSM-IV) diagnosis of psychiatric disorders, who were admitted and discharged between 2013-2015, which served as our broad inclusion criteria. Exclusion criteria were: age < 18 years; admitted into forensic unit; pregnant during inpatient stay; transferred to medical unit for medical intervention; or discharged after request for release by writing a 72-hour letter (a written request for discharge with 72 hours indicating the time the psychiatric hospital must discharge or seek retention) [23,27]. We could capture information on readmissions within 3 years to our facility only. Our clinician and social worker authors reviewed regulations and processes related to court-ordered psychiatric treatment and inpatient hospitalization [23-25].
3. Independent and Dependent Variables
We collected the following variables: demographic characteristics (e.g., age, gender, marital status, race/ethnicity, education, insurance, employment), clinical variables (e.g., psychiatric diagnoses, psychotropic medications, history of smoking, alcohol and drug use, medical comorbidities, sleep disturbance, history of psychiatric hospitalization), discharge disposition and follow-up care, and courtordered interventions or legal procedures: specifically, AOT, MOO, or retention for court.
For the definition of sleep disturbance, risk of suicide, and risk of violence, the assessment was primarily based on patients’ self-report along with clinicians’ judgement with or without an instrument, at time of admission. Specifically, if a patient is not sleeping for normal 6~8 hours with difficulty falling asleep or intermittent awakening, they were coded as having sleep disturbance. We used the Columbia Suicide Severity Rating for suicide risk assessment. Clinicians asked about suicidal ideation, suicidal behaviors, and patients responded “Yes/No” for each item of assessment. For risk of violence in the chart, we asked if patient has been violent, and patient responded “Yes/No”. We defined patients are at risk if they had violent behaviors. For psychiatric diagnosis and medical comorbidities, we followed the same or similar definitions and data sources, collection and documentation processes routinely followed, as done in [28]. Candidates for independent variables as possible predictors in the final, parsimonious multiple regression model were guided by the univariate association analyses of these variables and the study outcome, as described in the Statistical Analysis section.
The single dependent variable or primary outcome was LOS, determined by calculating the difference between date of admission and date of discharge. The median LOS was 14 days and used to categorize hospital stay as either longer vs. shorter than or equal to the median. Prolonged LOS was defined as longer than 30 days and was used for secondary or confirmatory purposes, the commonly accepted threshold in healthcare quality and policy literature along with readmission [29,30].
4. Statistical Analysis
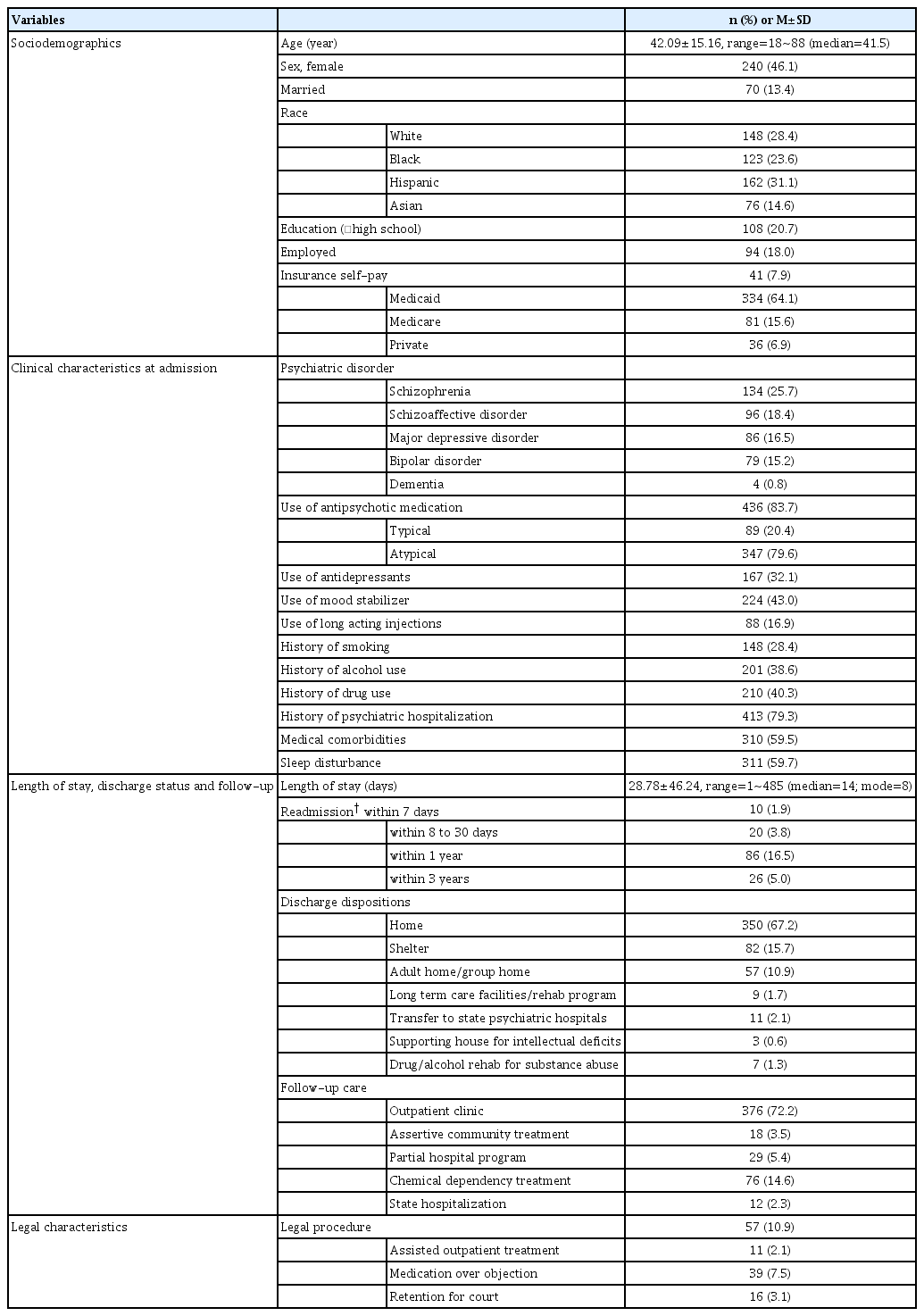
We used descriptive statistics to characterize study patients: mean and SD for continuous variables, additionally median, mode, and/or range when informative, and frequency and percentage for categorical variables. To compare the characteristics of patients with shorter vs. longer LOS, we used the x2 test or Fisher exact test for categorical variables without or with sparse data, respectively, and t-test for continuous variables between the two groups. Clinician authors selected potential covariates based on clinically meaningful factors supported by the literature and patient characteristics to avoid statistical significance (p-value)-driven association analyses. Specifically, Table 1 lists a comprehensive list to describe the study sample. Then Table 2 lists a reduced number of variables of our interest, including potential candidates for predictors of the outcome, and Table 3 shows the final set of predictors considered and fitted for the final regression models.
Simple and Multiple Logistic Regression Analysis for the Predictors of Longer and Prolonged LOS (N=521)
We evaluated associations between patient characteristics and longer LOS via logistic regression; unadjusted and adjusted odds ratios (ORs) were estimated via Simple and Multiple logistic regression, respectively, along with the corresponding 95% confidence intervals (CIs) and pvalues. For these models, we initially selected independent variables that showed a p-value <.1 in univariate associations between an independent variable and a dependent variable, without a sparse data issue, e.g., near zero count, in Table 2. These covariates are listed under “Unadjusted OR” in Table 3. Next, backward elimination was employed to reach a parsimonious model in multiple regression by deleting one covariate with the largest pvalue at a time until all covariates in the model reached p-value <.05 roughly, not strictly. We then double-checked that each of the omitted covariates was not statistically significant when added back to the final model; adjusted covariates are listed under “Adjusted OR” in Table 3. [Of note, we revised the final model based on a reviewer’s recommendation; changed age from continuous to categorical variable for easier interpretation. With this change, some covariates reached p=.06 so we kept them in the models.] We collapsed some categories to address sparse data issues, and we selected or derived one covariate among those that convey highly overlapping information based on scientific decision to avoid multicollinearity, non-estimability, or numerical instability of regression parameters, e.g., any legal procedure or none.
Next, we examined patient characteristics between the two subgroups - defined as with or without legal procedure - in a post-hoc, exploratory manner without formal comparison or testing, such that no p-values were computed or reported. Analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
1. Descriptive Statistics for Patient Characteristics
Among 521 psychiatric inpatients included in our study, mean/median LOS was 29/14 days, with a SD of 46 and a range of 1~485. Mean age was 42 years with a SD of 15 and a range of 18~88; 46% were female, 24% were Black, 31% Hispanic, and 15% Asian. Approximately 21% were educated beyond high school, and 18% employed. A total of 64% of patients were covered by Medicaid. With regard to psychiatric diagnoses, schizophrenia was most common (26%) and 84% of patients used antipsychotic medication. Almost 80% of patients had a previous psychiatric hospitalization and 60% had some medical comorbidity. Twentytwo percent of patients were readmitted to our hospital within 1 year, where approximately 6% (30/521) were readmitted to same inpatient psychiatric hospital within 30 days. Regarding discharge status, 67% were discharged to home, 16% to a shelter, and 11% to an adult or group home. Follow-up care was obtained at an outpatient clinic by 72% of patients and 15% received chemical dependency treatment. A total of 57 patients had intervention mandated by the courts: 11, AOT; 39, MOO; 16, retention, where two patients underwent both AOT and MOO, one patient had AOT and retention, and six patients experienced both MOO and retention. Table 1 provides a summary of patient characteristics including sociodemographic and clinical characteristics at admission, discharge status, follow-up care, and court-mandated status.
2. Sociodemographic, Clinical, And Legal Variables in Patients with Longer LOS vs. Shorter LOS
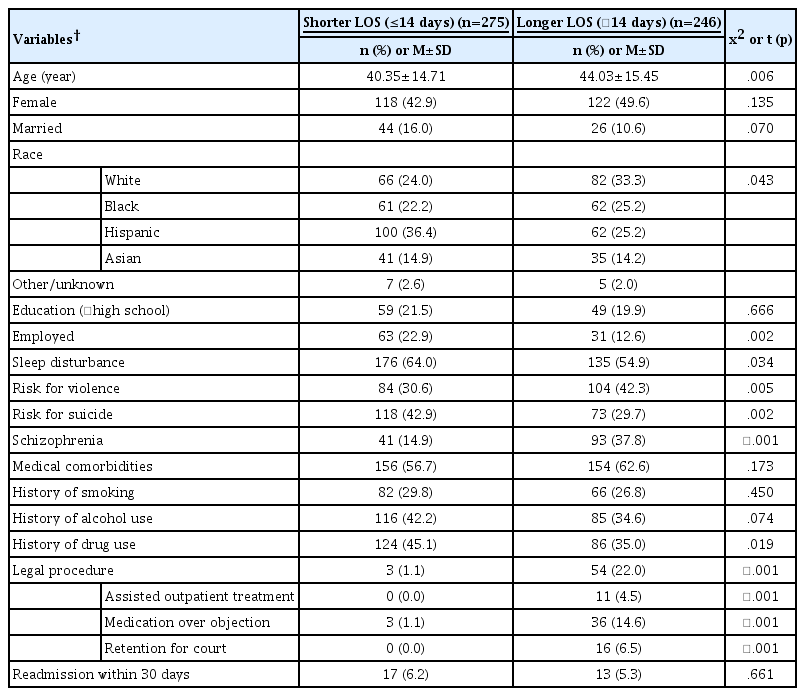
Table 2 summarizes patient characteristics according to shorter or longer LOS. A total of 246 (47.2%) patients of 521 had a longer LOS. In unadjusted association analyses, age, race, employment, sleep disturbance, risk of violence or suicide, schizophrenia, history of drug use, and any legal procedures were differentially distributed in the two groups; p<.05. Additionally, marital status and history of alcohol use showed weaker associations; .05<p<.10. These variables were considered for simple and multiple regression models. The 30-day readmission rate was not significantly different in the two groups (6.2% vs. 5.3%, p=.66).
3. Factors Associated with Longer and Prolonged LOS
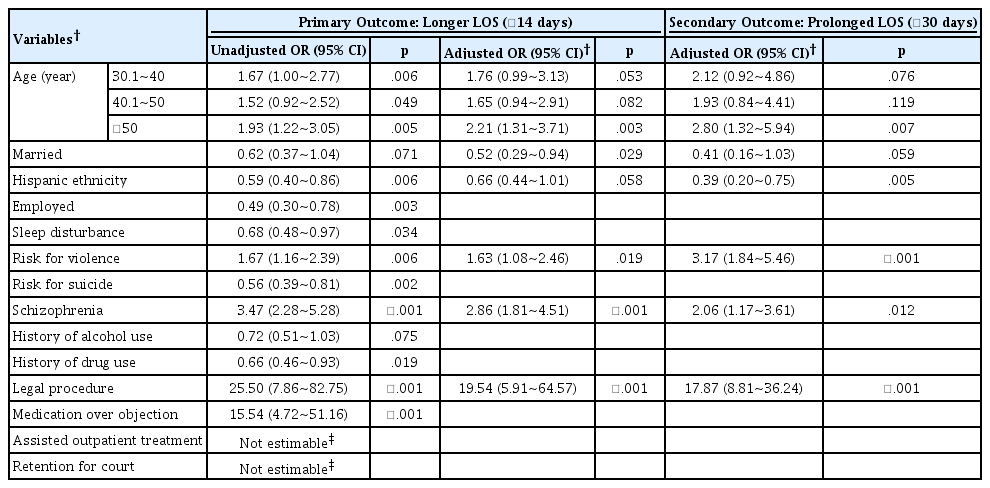
We evaluated associations between the 12 candidate covariates identified in the univariate association analyses with LOS (p<.1; Table 2), where unadjusted ORs for individual covariates were estimated in simple logistic regression; results are presented in Table 3. In the multiple regression analyses for adjusted ORs, the following six predictors were retained in the model for longer LOS: age; marital status; Hispanic ethnicity; risk of violence; schizophrenia; and court procedure. Being >50 years old at admission was associated with a longer LOS, compared to≤ 30 years old; OR=2.2 with 95% CI=1.3~3.7. Married or Hispanic patients tended to show a shorter LOS (OR=0.52; 95% CI=0.29~0.94 and OR=0.66; 95% CI=0.44~1.01, respectively). Patients who were at risk of violence or who had schizophrenia tended to have a longer LOS (OR=1.6; 95% CI=1.1~2.5 and OR=2.9; 95% CI=1.8~4.5, respectively). Consistent with results from the unadjusted association analyses, court procedure showed the strongest association; OR=19.5 with 95% CI=5.9~64.6. The two multiple regression models for longer and prolonged LOS showed qualitatively similar results overall with the same six predictors retained. For example, Hispanic ethnicity showed smaller OR further away from the null value (OR=0.39; 95% CI=0.20~0.75); this point estimate can be translated to 2.6 [=1/0.39] times increase in odds for non-Hispanic patients, for an easier comparison. The order of risk of violence and schizophrenia was reversed in the magnitude of the OR as well as the associated p-value.
4. Characteristics of Patients with or Without Legal Procedures
We described the characteristics of 57 patients with legal procedure vs. 464 patients without legal procedure, without formal comparison, e.g., no p-value or multivariable adjustment, as exploratory post-hoc analysis. Respectively, these groups differed in LOS; a mean of 78 vs. 23 days and a median of 63 vs. 13 days. Additionally, they were differences in alcohol use (18% vs. 41%), schizophrenia (51% vs. 23%), and discharge disposition (particularly, transfer to a state psychiatric hospital; 11% vs. 1%), respectively. Use of antidepressants and a diagnosis of major depressive disorder were notably lower among patients with versus without court involvement (5% vs. 35% and 0% vs. 19%, respectively). These results are presented in Table S1.
DISCUSSION
LOS and readmission rates in inpatient medical and psychiatric facilities have been studied for a few decades in the context of healthcare quality and policy, health outcomes, and services research. Given the current political and economic climate, there is even greater pressure to understand the causes and to contain costs [1-4]. Ensuring that patients with mental illness receive appropriate care is a particular challenge in the context of cost-benefit and efficiency, particularly since LOS is an important consideration for a variety of stakeholders: providers, hospital administrators, healthcare systems, government agencies, insurers, employers, patients, and families. Identifying factors associated with longer or prolonged LOS may help guide decisions made at time of admission, during inpatient care, and upon discharge.
Our study analyzed factors associated with LOS among 521 psychiatric inpatients. Longer LOS and legal procedures served as binary dependent and independent variables of primary interest. In contrast, most previous studies focused on patient-related factors including sociodemographic and clinical factors [5-22], hospital or regional characteristics [6,15-17,21], or provider- or service-related factors [18-22], less on legal factors. For example, some studies included legal status as a predictor of LOS but did not show the actual day information [6,21]; specifically, Compton et al. reviewed legal status at admission and at discharge, not court-ordered treatment. Zhang et al. included legal status, and it can be other than court-ordered treatments. Sood et al. evaluated characteristics that describe patients who are readmitted to an inpatient psychiatric hospital within one year of having their initial court order for treatment dropped with no subsequent mandated treatment; they reported that readmitted patients and a control group had 7.4 vs. 6.3 days, respectively, in rehospitalization for patients following release from courtordered evaluation [26]. Thus, these previous studies emphasized topics different from the court-ordered treatment.
In contrast, Russ and John can be viewed more directly relevant to the current study [24]. Their and our findings are qualitatively similar, but these two studies were based on different study designs with somewhat different focuses. LOS was studied for exploratory analyses with summary statistics only in Russ and John; they reported a mean LOS of 82 days among 130 patients with the MOO status vs. 50 days in a comparison group of 89 patients who transiently refused medication vs. 29 days in a control group of 132 patients who agreed to treatment [24]. To compare, our study performed this comparison as a prespecified primary hypothesis with a more precise estimation of LOS and associational measures with multi-variable adjustment. Then we found that older age, being unmarried, of non-Hispanic ethnicity, at risk of violence, a diagnosis of schizophrenia, and court involvement showed longer LOS in the final adjusted regression models, with broader court involvement demonstrating the most pronounced association.
Based on our more definitive or confirmatory study (after an earlier, initial report by Russ and John), the psychiatry literature and communities may consider court-ordered psychiatric intervention or other legal procedures as a key factor in hospital LOS estimation or prediction. Providers, administrators, and discharge planners might use it to inform treatment schedule, predict LOS, or build in efforts to reduce readmission and LOS in this high-risk population, who are often noncompliant with medication after discharge, refractory to treatment, or out of touch with the healthcare system. Also, legal variables may be placed in a prominent place in the “variable importance” literature on psychiatric LOS, e.g., top 3 or 10 predictors [6,21].
Some limitations of this study should be noted. First, this study was based on a retrospective chart review with well-known inherent limitations. Only variables that were recorded and available could be utilized; we had no control over incomplete or error-prone data, such as occurs in self-reported information already recorded. Although we used group consensus for data retrieval and verification, we did not formally assess consistency among the data abstractions or inter-rater reliability in our low budget study; yet we followed similar approaches used in [28]. We also could not access readmission data from facilities other than our medical center. Second, data on disease severity, age of onset of psychiatric illness, level of family or social support, living situation, and cultural characteristics were not available, but could be potential confounders or mediators. We were also unable to study clinician-level factors either. Third, as a single site study in one country, it could have limited generalizability and we could not study hospital or institutional characteristics or differences in different hospital or legal practices. Future studies may aim to answer an important question that carries policy or practice implications could be whether discharge disposition (referral to state hospital, nursing home, rehabilitation, or group home) leads to shorter hospital stays for those who await an opening while in psychiatric hospitals. Finally, our data are relatively old, with possible limitations to current clinical practice, although we are not aware of notable practice or policy changes directly relevant to our research for the last five years. However, we would be interested in the potential impacts of the Affordable Care Act and COVID-19 on psychiatric hospital system as future research.
Our study has some strengths. We included multi-year data from a large urban medical center that represents a diverse population, including 15% Asians. Also, we were able to study and document data less commonly reported in the literature, such as type of court-mandated intervention. Information pertaining to court status entailed authors’ careful reading of legal documentation and crosschecking it with inpatient hospital records, along with ensuing group discussion. Additionally, our study's relatively large sample size of its kind based on a systematic sampling may provide a reasonable estimate of the prevalence of key variables; e.g., 11% presence of court involvement; roughly 50%/20% patients with longer than 14/30 days in hospital; and 6% readmission, that case-control or convenient samples used in previous studies may not offer readily.
CONCLUSION
We found that variables reflecting court-mandated psychiatric interventions or legal procedures such as AOT, MOO, and retention showed a strong association with longer psychiatric hospital LOS relative to sociodemographic and clinical factors, even after multi-variable adjustment. Patients with legal procedure had substantially longer LOS (more than 3 times by mean or median), compared to those without. These factors may not be routinely considered in the general LOS research and current clinical practice. For example, if mental health clinicians figure out that their patients need legal procedure when they are admitted, they may apply AOT or proceed MOO right away instead of waiting for patients to take medications or wasting time. That way, patients may not need to stay long by waiting for court order during inpatient hospitalization; early recognition and intervention may prevent longer stay. Legal procedures may be emphasized in psychiatric settings as a possible aid or a key factor in inpatient and community care, toward enhanced monitoring, surveillance and support services in this high-risk group.
Notes
The authors declared no conflicts of interest.
AUTHOR CONTRIBUTIONS
Conceptualization or/and Methodology: Shin J & Bang H
Data curation or/and Analysis: Ho-Periola A & Ramer S & Kwon Y & Bang H
Funding acquisition: Shin J
Investigation: Shin J & San Gabriel MC & Ho-Periola A & Ramer S & Bang H
Project administration or/and Supervision: Shin J & Bang H
Resources or/and Software: Shin J & San Gabriel MC & Bang H
Validation: Kwon Y & Bang H
Visualization: N/A
Writing: original draft or/and review & editing: Shin J & San Gabriel MC & Ho-Periola A & Ramer S & Kwon Y & Bang H
Supplement
Comparison of Patients with or without Legal Procedures